Rheumatoid Arthritis of Knee: Causes, Symptoms and Treatments
Imagine waking up every morning with excruciating pain in your knees, making it difficult to even get out of bed. For millions of people worldwide, this is a daily reality due to a condition known as rheumatoid arthritis of knee. This debilitating autoimmune disease not only causes severe joint pain and swelling but can also lead to permanent damage and disability if left untreated.
In this article, we will delve into the intricacies of rheumatoid arthritis, specifically affecting the knee joint, exploring its symptoms, causes, diagnosis, and treatment options. Whether you are someone living with this condition or simply seeking to understand it better, join us on a journey to unravel the complexities of rheumatoid arthritis of the knee and discover how it impacts the lives of those affected by it.
Contents
- 1 Understanding Rheumatoid Arthritis of the Knee
- 2 Understanding the Knee Joint Anatomy
- 3 Causes of Rheumatoid Arthritis in Knees
- 4 Identifying Symptoms of Rheumatoid Arthritis
- 5 Diagnosis Process for Rheumatoid Arthritis
- 6 Treatment Options for Knee Rheumatoid Arthritis
- 7 Living with Rheumatoid Arthritis: Lifestyle Adjustments
- 8 FAQ’s
- 8.1 What is the best treatment for rheumatoid arthritis in the knees?
- 8.2 What are the four stages of osteoarthritis in the knee?
- 8.3 What are the three symptoms of rheumatoid arthritis?
- 8.4 How do you know if you have arthritis in your knee?
- 8.5 What does rheumatoid arthritis feel like in the knees?
- 8.6 What are the four stages of osteoarthritis in the knee?
- 8.7 What does arthritis in the knee feel like?
- 8.8 What is the best thing to take for arthritis in your knees?
- 9 Conclusion: Rheumatoid Arthritis of Knee
Understanding Rheumatoid Arthritis of the Knee

Effective management of rheumatoid arthritis in the knee requires a comprehensive approach that combines medication, physical therapy, lifestyle modifications, and possibly surgery. Early intervention with disease-modifying antirheumatic drugs (DMARDs) can help slow or halt disease progression by suppressing inflammation and preventing further joint damage. Furthermore, regular low-impact exercises such as swimming or cycling can strengthen surrounding muscles while minimizing stress on the affected knees. In more severe cases where conservative measures prove ineffective, surgical options like arthroplasty may be necessary to restore functionality and alleviate pain.
Understanding the Knee Joint Anatomy
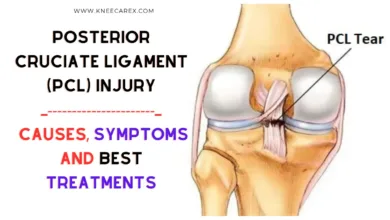
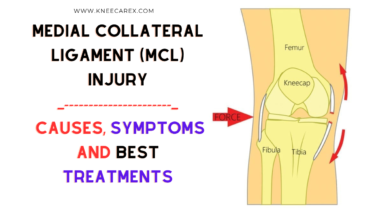
The knee joint is a marvel of engineering, comprising complex structures that allow for movement while bearing the body’s weight. At its core, the knee joint consists of the articulation between three bones: the femur (thigh bone), tibia (shinbone), and patella (kneecap). These bones are held together by a network of ligaments, including the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL), which provide stability and control movement within the joint. Additionally, the meniscus, a cartilaginous structure located between the femur and tibia, acts as a shock absorber to cushion impact during activities such as walking or running.
Understanding the intricate anatomy of the knee joint allows for a deeper appreciation of its vulnerability to conditions such as rheumatoid arthritis. The synovial membrane, which lines the inner surface of the joint capsule, can become inflamed in rheumatoid arthritis, leading to pain, swelling, and damage to surrounding tissues. Furthermore, understanding how different parts of the knee joint function together provides valuable insight into potential treatment options for managing rheumatoid arthritis symptoms. By delving into this anatomical complexity, we can gain greater empathy for those living with knee-related challenges and develop more effective strategies for addressing their needs.
Causes of Rheumatoid Arthritis in Knees

Hormonal changes, particularly in women, have been observed to play a role in the development of RA in knee joints. Estrogen fluctuations have been linked to increased susceptibility to autoimmune diseases, including rheumatoid arthritis. Additionally, recent research suggests that gut health may be linked to the development of RA, with imbalances in gut bacteria potentially contributing to the inflammation seen in knee joints affected by RA. Understanding these underlying causes could lead to more targeted treatments for managing and preventing rheumatoid arthritis, specifically affecting the knees.
Fractures (Patellar Femoral and Tibial): Causes, Symptoms and Treatments
Identifying Symptoms of Rheumatoid Arthritis
Identifying the symptoms of rheumatoid arthritis can be challenging, as they often mimic other joint-related conditions. However, there are key indicators that may point to the presence of this chronic autoimmune disorder. One significant symptom is morning stiffness lasting more than an hour, particularly in the joints. Additionally, noticeable swelling, warmth, and tenderness around the affected joints could signal the onset of rheumatoid arthritis.
Rheumatoid arthritis also manifests itself through systemic symptoms such as fatigue, fever, and weight loss. These non-specific symptoms may not immediately raise suspicion for arthritis but should not be dismissed if accompanied by joint discomfort. It’s essential to pay attention to any changes in joint function or flexibility that persist beyond a few weeks, as early detection and treatment can significantly improve long-term outcomes for those living with this condition.
Diagnosis Process for Rheumatoid Arthritis

Best Radiologists for X-rays and ultrasounds near You
Furthermore, diagnosing RA often requires a multidisciplinary approach involving working collaboratively with rheumatologists, orthopedic surgeons, and primary care providers. This coordinated effort allows for a comprehensive assessment of symptoms, joint function, and overall health status. Moreover, as new diagnostic technologies emerge, such as ultrasound and advanced imaging techniques, the ability to detect early signs of RA has significantly improved. Early diagnosis is paramount in managing the disease effectively and preventing long-term joint damage—a crucial point that patients should actively consider when seeking medical attention for suspected RA symptoms.
Treatment Options for Knee Rheumatoid Arthritis
When it comes to treating knee rheumatoid arthritis, there are several options available that can help manage pain and improve function. One such option is medication, which may include nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), or biologic agents. These medications can help reduce inflammation, slow the progression of the disease, and alleviate discomfort in the knee joint.
Physical therapy is another crucial aspect of treatment for knee rheumatoid arthritis. Working with a physical therapist can help patients improve their knee’s range of motion, strength, and flexibility through targeted exercises and stretches. Additionally, assistive devices such as braces or walking aids may be recommended to reduce stress on the affected knee joint during daily activities. In some cases, surgical interventions like joint replacement surgery may be considered when other treatments have not provided sufficient relief for severe cases of knee rheumatoid arthritis. These treatment options offer hope to those dealing with this condition by providing practical ways to manage symptoms and maintain an overall quality of life.
Living with Rheumatoid Arthritis: Lifestyle Adjustments

In addition to exercise, adopting a well-balanced diet rich in anti-inflammatory foods like fruits, vegetables, and healthy fats can positively impact managing rheumatoid arthritis symptoms. Many individuals with rheumatoid arthritis also benefit from making ergonomic changes to their living spaces, such as using assistive devices in the kitchen or bathroom to ease daily tasks on the joints. These lifestyle adjustments not only help alleviate the physical challenges of rheumatoid arthritis but also provide a sense of empowerment over the condition.
FAQ’s
What is the best treatment for rheumatoid arthritis in the knees?
Rheumatoid arthritis in the knees is treated using a multidisciplinary approach, including medications, physical therapy, and biological therapy. Physical therapy helps maintain knee function and mobility, while corticosteroid injections may be recommended for pain relief. Lifestyle modifications like maintaining a healthy weight, engaging in low-impact exercises, and using assistive devices can also help manage symptoms and prevent further deterioration.
What are the four stages of osteoarthritis in the knee?
The four knee osteoarthritis stages are a significant determinant of symptom severity and treatment approach. In the initial stage, the knee cartilage shows signs of wear and tear, leading to mild discomfort and occasional pain during movement. As the condition progresses to stage two, there is evident cartilage loss, resulting in increased pain, stiffness, and reduced range of motion in the affected knee. This is often accompanied by inflammation and noticeable changes in imaging, such as X-rays or MRIs.
What are the three symptoms of rheumatoid arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune condition affecting various joints, including the knees. Key symptoms include persistent joint pain, swelling, stiffness, and inflammation. This can impact mobility and the quality of life. Patients may also experience warmth and redness around the affected joint. Additionally, RA can increase fatigue levels, making daily activities more challenging.
How do you know if you have arthritis in your knee?
One of the first signs of arthritis in the knee is persistent pain and stiffness, especially when getting up from sitting or after periods of inactivity. Many people with knee arthritis also experience joint swelling, making it difficult to bend or straighten the knee fully. In some cases, a grating sensation or a clicking sound may accompany movement in the affected knee, indicating potential damage to the joint’s cartilage.
What does rheumatoid arthritis feel like in the knees?
The sensation of rheumatoid arthritis in the knees is often challenging to put into words. It’s like a relentless, deep ache that never goes away, combined with bursts of sharp pain that feel like your knees are being twisted and pulled from the inside. The stiffness is also overwhelming; it’s as if your knees have been encased in concrete, making even simple movements challenging. Walking becomes an Olympic feat, and each step feels like a battle against invisible forces determined to keep you immobile.
What are the four stages of osteoarthritis in the knee?
Osteoarthritis is a debilitating condition that affects millions of people worldwide, causing pain and limitations in mobility. In the knee, osteoarthritis progresses through four stages, each presenting unique challenges for patients and healthcare providers. The first stage involves minor damage to the cartilage, often accompanied by occasional pain or discomfort during activity. As the condition advances to the second stage, there is noticeable thinning and roughening of the cartilage, leading to increased pain and stiffness.
What does arthritis in the knee feel like?
Imagine waking up in the morning with a dull, persistent ache in your knee that makes every step feel like a monumental effort. For those living with arthritis in the knee, this is an all-too-familiar experience. The joint feels stiff and swollen as if resisting movement at every turn. The pain can range from mild discomfort to sharp, shooting sensations that make simple tasks like climbing stairs or bending down excruciating.
What is the best thing to take for arthritis in your knees?
As one of the primary weight-bearing joints in the body, knees affected by arthritis can cause significant pain, stiffness, and reduced mobility. So, what is the best thing to take for arthritis in your knees? While there is no one-size-fits-all answer, many people find relief through a combination of treatments such as prescription medications, physical therapy, and lifestyle modifications. One common medication used to manage knee arthritis is nonsteroidal anti-inflammatory drugs (NSAIDs), which help reduce pain and inflammation. Physical therapy can also play a crucial role in strengthening muscles around the knee joint and improving overall function.
Conclusion: Rheumatoid Arthritis of Knee
In conclusion, managing and treating rheumatoid arthritis of the knee requires a comprehensive approach that combines medication, physical therapy, and lifestyle changes. Patients must work closely with their healthcare team to find the most effective treatment plan for their needs. This may involve trying different medications or therapies to find the right combination that provides relief and improves mobility.