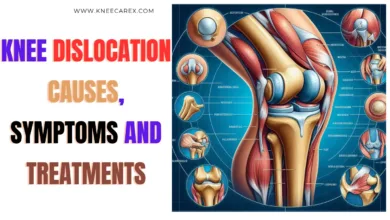
Knee Rheumatoid Arthritis: Causes, Symptoms and Treatments
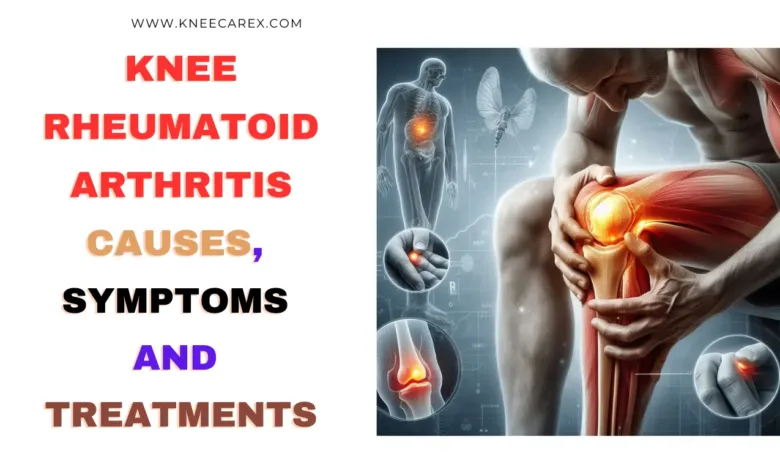
Knee Rheumatoid arthritis is a severe and persistent illness that affects millions of people worldwide. While it can strike any joint, the knee is often a primary target, leading to excruciating pain, stiffness, and limited mobility. In this article, we will delve into the intricate web of causes behind rheumatoid arthritis of the knee, unravel its telltale symptoms, and explore the myriad treatment options available to alleviate its impact on daily life.
Contents
- 1 Understanding Rheumatoid Arthritis of the Knee
- 2 What Triggers Rheumatoid Arthritis in Knees?
- 3 Identifying Signs of Knee Rheumatoid Arthritis
- 4 How is rheumatoid arthritis of the knee detected?
- 5 Modern and Traditional Approaches
- 6 Living with Rheumatoid Arthritis: Coping Strategies
- 7 FAQ’s
- 7.1 What are the seven signs of rheumatoid arthritis?
- 7.2 What does rheumatoid arthritis in the knee feel like?
- 7.3 What are the four stages of osteoarthritis in the knee?
- 7.4 What can you do for rheumatoid arthritis in the knee?
- 7.5 How do I know if I have osteoarthritis or rheumatoid arthritis?
- 7.6 How do I know if my knee pain is rheumatoid arthritis?
- 7.7 Can an X-ray show the difference between osteoarthritis and rheumatoid arthritis?
- 7.8 What are the seven diagnostic criteria for RA?
- 7.9 What does rheumatoid arthritis in the knee feel like?
- 7.10 What are the seven signs of rheumatoid arthritis?
- 7.11 What is the first thing to do when you have rheumatoid arthritis?
- 7.12 Does rheumatoid arthritis hurt every day?
- 7.13 What is the best treatment for arthritis in the knee?
- 7.14 What is the best home remedy for knee arthritis?
- 7.15 Is walking good for knee arthritis?
- 7.16 What is the best exercise for arthritic knees?
- 8 Conclusion: Rheumatoid Arthritis of the Knee
Understanding Rheumatoid Arthritis of the Knee

As we delve into this topic, we will unravel the intricate web of factors contributing to the development of rheumatoid arthritis in the knee joint, from genetic predispositions to environmental triggers. Furthermore, we will shed light on the array of symptoms experienced by those with rheumatoid arthritis in their knees, ranging from persistent swelling and stiffness to difficulty bearing weight on the affected leg. Lastly, we will examine conventional and cutting-edge treatment approaches, such as medication management, physical therapy interventions, and surgical techniques, to reduce symptoms and enhance general knee joint function in individuals with rheumatoid arthritis.
What Triggers Rheumatoid Arthritis in Knees?
The complicated autoimmune condition known as rheumatoid arthritis (RA) can affect multiple joints, including the knees. The exact triggers for RA in the knees are not fully understood, but they are thought to be a result of a mix of environmental and genetic influences. An overactive immune system mistakenly attacks the synovium, the lining of the knee joint, leading to inflammation, pain, and eventual damage to the joint.
Researchers are exploring various potential triggers for RA in the knees, such as smoking, obesity, and hormonal factors. There is substantial evidence connecting smoking to a higher risk of developing RA and that it may also exacerbate symptoms in those who already have the condition. Additionally, carrying excess weight puts extra stress on the knee joints, potentially worsening inflammation and accelerating joint damage. Hormonal changes or imbalances in women have furthermore been connected to an increased risk of getting or flare-ups of RA.
Choosing the Right Support: Patella Band vs Knee Sleeve for Knee Pain Relief
Identifying Signs of Knee Rheumatoid Arthritis

Another essential sign to watch for is a reduced range of motion in the knee that is injured. This can manifest as difficulty fully extending or bending the knee, leading to mobility issues and discomfort during daily activities. Furthermore, if you notice redness over the skin covering the knee joint, these symptoms could indicate an active flare-up of rheumatoid arthritis in the knee. Early detection of these symptoms can result in timely intervention and better management of this condition.
How is rheumatoid arthritis of the knee detected?
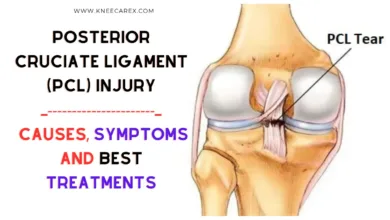
Rheumatoid arthritis (RA) of the knee is often detected through medical history, physical examination, and imaging tests. During the medical history, the doctor will inquire about any pain, swelling, stiffness, and limitations in movement experienced in the knee. The physical examination involves assessing the affected knee for warmth, tenderness, and signs of inflammation, such as redness or swelling.
To verify the diagnosis and assess the severity of joint damage caused by RA, imaging tests like X-rays and MRIs are utilized. X-rays can reveal joint erosion, narrowing of shared space, or bone deformities—all typical indicators of RA. Meanwhile, MRIs provide detailed images that aid in identifying soft tissue changes around the joint and detecting early signs of inflammation not visible on X-rays. These diagnostic methods help healthcare professionals see RA early so appropriate treatment plans can be initiated to minimize long-term joint damage and improve patients’ quality of life.
Modern and Traditional Approaches
In rheumatoid arthritis (RA) treatment for the knee, there is a constant debate between modern and traditional approaches. Current therapies, such as biologic drugs and disease-modifying antirheumatic drugs (DMARDs), offer targeted relief by addressing the underlying causes of inflammation. On the other hand, traditional remedies like physical therapy and lifestyle modifications focus on holistic approaches to managing pain and improving joint function.
While modern treatments may be at the forefront of medical advancements, traditional approaches have stood the test for their long-term effectiveness and minimal side effects. In some cases, combining both methods can lead to a comprehensive approach to managing RA in the knee. By considering modern and traditional approaches, patients can collaborate with their medical professionals to develop a customized treatment plan that addresses their unique needs while minimizing potential risks.
Living with Rheumatoid Arthritis: Coping Strategies

It’s also essential for individuals living with rheumatoid arthritis to build a strong support network. This may include connecting with others who have the condition through support groups or online communities and educating friends and family members about the challenges of living with rheumatoid arthritis. Finally, staying informed about the latest treatment options and advancements in research can empower individuals to take an active role in their care and advocate for the best possible outcomes. By employing these coping strategies, individuals with rheumatoid arthritis can enhance their quality of life and foster a sense of resilience in the face of their condition.
FAQ’s
What are the seven signs of rheumatoid arthritis?
Rheumatoid arthritis is characterized by joint pain, stiffness, fatigue, limited mobility, morning stiffness, fever, and weight loss. These symptoms can be triggered by inactivity, causing difficulty in daily tasks and affecting motivation for exercise or socializing. Recognizing these signs can help individuals seek early intervention and consult healthcare professionals for a personalized treatment plan. A higher quality of life and better results can result from early detection.
What does rheumatoid arthritis in the knee feel like?
Rheumatoid arthritis in the knee is a severe, persistent pain that can be intense and limiting. It can cause a constant sense of unease and dependency on others. Simple movements can trigger pain, making every step an endurance challenge. The condition also causes emotional strain, leading to feelings of isolation and helplessness. Despite these challenges, managing this condition can provide hope and empower individuals to live fulfilling lives.
What are the four stages of osteoarthritis in the knee?
Osteoarthritis in the knee progresses through four stages: early, moderate, severe, and end-stage. The early stage involves minor cartilage damage and inflammation, while the intermediate stage leads to increased pain, swelling, and reduced mobility. The severe stage involves significant cartilage deterioration, deformity, and chronic pain; the end stage results in irreversible damage, necessitating surgical intervention like a total knee replacement.
What can you do for rheumatoid arthritis in the knee?
Living with rheumatoid arthritis in the knee can seem like a difficult task, but there are a few things you can do to control the illness and raise your standard of living. One of the first and most important things to do is work closely with a healthcare expert to create a thorough treatment plan customized to your needs. This could involve a mix of prescription drugs, physical therapy, and lifestyle changes. Modifications are designed to reduce inflammation, alleviate pain, and improve joint function.
How do I know if I have osteoarthritis or rheumatoid arthritis?
It is essential to comprehend the distinctions between rheumatoid arthritis and osteoarthritis to receive an early diagnosis and proper treatment. Osteoarthritis causes pain and stiffness, while rheumatoid arthritis causes joint inflammation and deformity. Symptoms like morning stiffness and symmetrical joint involvement can distinguish between the two. Systemic symptoms, like fatigue and fever, are also significant. Blood tests for specific antibodies can confirm a rheumatoid arthritis diagnosis.
How do I know if my knee pain is rheumatoid arthritis?
Determining whether your knee pain is due to rheumatoid arthritis (RA) can be challenging as it shares symptoms with other conditions. The primary differentiator is the existence of other RA symptoms, such as joint stiffness, swelling, and warmth. Additionally, RA typically affects joints symmetrically and can cause fatigue, fever, and weight loss. A thorough evaluation from a healthcare professional is crucial for an accurate diagnosis. Furthermore, undergoing specific blood tests and imaging studies can help confirm the presence of RA markers in the body.
Can an X-ray show the difference between osteoarthritis and rheumatoid arthritis?

What are the seven diagnostic criteria for RA?
To correctly diagnose and treat rheumatoid arthritis (RA), an intricate autoimmune illness, one must adhere to seven diagnostic criteria. First and foremost, joint involvement is an important marker, mainly if it affects three or more joints at once. Second, the length of the symptoms needs to be assessed; chronic joint pain and stiffness lasting at least six weeks is a crucial component. Furthermore, rheumatoid nodules found beneath the skin may provide additional evidence in favor of an RA diagnosis.
What does rheumatoid arthritis in the knee feel like?
Imagine waking up one morning and feeling an intense, throbbing pain in your knee that radiates with every step you take. This is just a glimpse of what it feels like to have rheumatoid arthritis in the knee. The sensation can be likened to a relentless ache that gnaws at the joint, making even simple movements excruciatingly painful. Many describe it as a persistent, deep-seated discomfort that refuses to relent, no matter how much rest or medication is taken.
What are the seven signs of rheumatoid arthritis?
Rheumatoid arthritis is a chronic condition characterized by persistent fatigue, joint pain and swelling, morning stiffness, intermittent low-grade fevers, numbness or tingling in the hands and feet, decreased range of motion due to joint inflammation, and loss of appetite. These symptoms can significantly impact daily life, mobility, and the ability to perform tasks effectively. The disease’s multifaceted nature highlights its potential impact on physical health and well-being. To properly treat the symptoms of rheumatoid arthritis, one must be aware of its indications and symptoms.
What is the first thing to do when you have rheumatoid arthritis?
The first essential step when diagnosed with rheumatoid arthritis is to consult a knowledgeable rheumatologist. Establishing a trustworthy healthcare team that understands the complexities of this condition and can offer tailored treatment plans is crucial for managing the symptoms effectively. Additionally, seeking support from fellow individuals dealing with rheumatoid arthritis through support groups or online communities can provide invaluable emotional and practical guidance.
Does rheumatoid arthritis hurt every day?
One autoimmune chronic disease that causes rheumatoid arthritis is causes joint pain, inflammation, and stiffness. While it varies from person to person, many individuals with rheumatoid arthritis do experience daily pain. This can be due to the ongoing inflammation and joint damage caused by the immune system’s attack on the body’s tissues. The severity of the pain may fluctuate, but for some individuals, it is indeed a constant presence in their lives.
What is the best treatment for arthritis in the knee?
The best treatment for knee arthritis depends on the severity and individual needs. Mild cases can be treated with non-invasive physical therapy and weight management methods. A combination of treatments may be needed for advanced patients, including platelet-rich plasma therapy and stem cell therapy. Personalized care plans and consulting with orthopedic professionals are crucial for effective treatment.
What is the best home remedy for knee arthritis?
As knee arthritis continues to be a common ailment affecting millions, the search for effective home remedies becomes increasingly essential. One particularly promising remedy gaining attention is turmeric. This golden spice contains curcumin, a powerful anti-inflammatory compound that may help reduce the pain and swelling associated with arthritis. For some people with knee arthritis, adding turmeric to their diet or taking it as a supplement may provide relief.
Is walking good for knee arthritis?
Despite commonly being associated with high-impact activities, walking is beneficial for knee arthritis. Contrary to popular belief, walking can help bolster the knee joint’s supporting muscles and enhance flexibility, ultimately reducing pain and stiffness. Regular walking can also contribute to weight management, alleviating pressure on the knees and diminishing discomfort. Moreover, studies have suggested that engaging in moderate-intensity walking may even slow down the progression of knee arthritis by promoting better joint function and reducing inflammation.
What is the best exercise for arthritic knees?
When finding the best exercise for arthritic knees, it’s essential to prioritize low-impact activities that still provide a great workout. Swimming often tops the list as an ideal exercise for those with knee arthritis, as it allows for fluid movement without putting excess strain on the joints. The water supports the body and provides resistance, helping to strengthen muscles around the knees while minimizing impact.
Conclusion: Rheumatoid Arthritis of the Knee
In conclusion, knee rheumatoid arthritis is a complex and debilitating condition that significantly impacts the quality of life for those affected. Patients must work closely with healthcare professionals to create a thorough treatment strategy that takes into account the disease’s symptoms and underlying causes. Additionally, lifestyle modifications such as regular exercise, weight management, and joint protection techniques can complement medical interventions in managing knee rheumatoid arthritis.